Fulfilling Robin’s Wish
The iconic house on Steiner and Broadway in San Francisco draws lively crowds of tourists. Fragrant roses line its edges and blooming wisteria climbs to the corners of the curtained windows. Excited visitors stand near the iron gates, flashing big smiles for photos, while others wait in anticipation, staring at the house as if Mrs. Doubtfire is about to greet them at the door with a plate of warm cookies. However, the property is just a prop from the beloved 1990s film starring Robin Williams as a transformed dad-turned-nanny. Even though it’s all imaginary, we still can’t help but envision Robin Williams bouncing down the steps humming a catchy tune as the movie’s title character, nor do we want to accept that our cherished Robin Williams is gone, never to brighten us with his witty humor and piercing blue eyes.
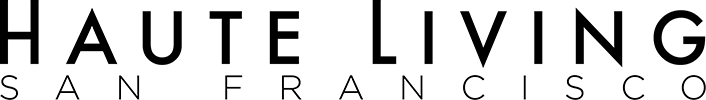
Robin Williams’ characters provided a sense of purpose and insight into life’s questions for so many individuals, while his comedy brought joy to countless people around the globe. With the many roles he played that spoke to us, it felt as though we knew him personally, but only one person truly knew him, that was his wife, Susan Schneider Williams. As a beloved comedian and actor, Robin Williams’ impact was immeasurable, but now in his death, his widow gives Robin’s legacy meaning.
Susan Schneider Williams shares, “We met each other at just the right time in both of our lives. We had been through enough that we appreciated each other. We both valued respect and unconditional love. I never wanted to change Robin. I got clean and sober at age 20, and we had that in common. Our commitment to clean living and honesty was our connecting point, and we were a safe harbor for each other. I never had that shelter until I met Robin. Robin used to call me his warrior princess, and he made me feel like a princess.”
Before being catapulted into the media following Robin’s death, Susan had a successful career as a graphic designer and artist. After completing her studies at California College of the Arts, she spent 25 years as a graphic designer specializing in identity design, corporate branding, and marketing. For the last 15 years of her design career, she ran her company, Critical Eye Design. Susan indulged her love for painting in her free time, losing herself in expression and discovery. In 2006, she began turning her passion for fine art into a full-time career, transitioning from design to focus exclusively on painting and thus founding Susan Schneider Fine Art.

Susan’s passion for art extends beyond her paintings. In addition to creating beautiful pieces inspired by the Impressionists, Hudson River School artists, and John Singer Sargent, she has experience as an accomplished mentor, private teacher, and curator. Her talent for sharing her skills and vision with fellow artists has enriched her career and led to numerous exhibitions, group and solo, and her work being held in private collections worldwide.
But that all changed on August 11, 2014.
It felt as if the world stopped spinning and an awful prank was being played on every news station across the world.
“Robin Williams is dead at the age of 63 by apparent suicide.”
Susan lost her husband, her confidant, the love of her life, and her safe harbor.

“After his death, he wasn’t there to protect me anymore, and I had to protect both of us. I didn’t ask why. Why is a ridiculous question. In most cases, it’s the how. I was the boots on the ground now trying to understand what killed my husband,” Susan shares.
THE BEGINNING OF THE END
Susan takes us back to when Robin first showed mysterious symptoms: “I was busy painting and working, then my husband started having these random anxieties and sleeping problems. We were chasing symptoms, trying to get to the bottom of what was going on. What I know now is there are over 40 symptoms of the disease that took his life. We didn’t know they were all connected, and none of the doctors knew.”
She continues, “In October 2013, 10 months before his passing, Robin sought medical attention for a range of seemingly unrelated symptoms, including constipation, urinary difficulty, heartburn, sleep disruptions, and a diminished sense of smell. While under great stress, he also experienced intermittent tremors in his left hand that were initially attributed to a past injury. Despite ongoing care from his doctors, his health declined.”
Despite testing negative for diverticulitis, Robin Williams experienced various symptoms that seemed to come and go randomly. Over the next 10 months, these symptoms increased in severity and frequency, making them difficult to manage. By winter, he was experiencing problems with paranoia, delusions, looping, insomnia, memory, and high cortisol levels. Seeking medical help and psychotherapy became a constant as he tried to manage these seemingly unrelated conditions.
In April 2014, while filming Night at the Museum 3 in Vancouver, Robin experienced a panic attack. He struggled to remember even one line for his scenes, despite performing flawlessly in a 5-month Broadway production three years earlier. This sudden loss of memory and inability to manage his anxiety deeply upset him.

“Despite numerous doctor appointments, testing, and psychiatry sessions, he repeatedly expressed his desire to ‘reboot’ his brain. We underwent an excessive number of blood tests, urine tests, and cortisol and lymph node checks, as well as a brain scan and cardiac exam. While the results of all these tests were negative, his cortisol levels persistently remained high. Though we were relieved to hear the test results were negative, Robin and I were both left with an uneasy feeling that something was deeply wrong. Finally, on May 28, he was diagnosed with Parkinson’s disease,” Susan recalls.
“We thought we figured it out once we got a diagnosis of Parkinson’s, but Robin knew that there was something more going on.”
Susan felt relieved when Robin finally received a diagnosis of Parkinson’s disease. However, she soon realized that he wasn’t himself and was slowly losing his confidence, becoming obsessed with inconsequential things. “It was like watching a loved one drown in quicksand, helpless to do anything. The real diagnosis finally came after Robin’s death, which was a devastating blow,” she admits.
It was too late to save Robin Williams, but Susan became determined to raise awareness about the devastating illness that took Robin’s mind in hope she could save others from the devastating experience she and her husband endured.
“I felt like I was hearing the name of my husband’s killer for the first time.”
While Robin was alive, medical experts could not diagnose the root of his suffering, there was no biomarker for an accurate diagnosis. At the time of his death, only autopsies could confirm that he had Lewy body dementia.
Lewy body dementia is a medical condition where normal proteins, called alpha-synuclein, become misfolded and build up in the brain. These misfolded proteins, known as Lewy bodies, interfere with the brain chemicals responsible for mental function, physical movement, behavior, and mood.
These deposits of abnormal proteins interfere with regular brain activity and can lead to various dysfunctions, including emotional, cognitive, and motor imbalances.
“No medical professionals had it figured out. What I know now is that Robin’s Parkinson’s diagnosis was incomplete. It was the end of Robin’s disease progression, not the beginning,” Susan explains.
Nearly every region of his brain and brainstem was riddled with these abnormal alpha-synuclein protein deposits. For Susan, the mere fact that something had invaded almost every part of her husband’s brain made perfect sense to her.
“I know my husband was struggling, and it took everything for Robin to make it through the day. So, after his death, finally having an accurate diagnosis, I sought to understand this disease.”
After a thorough brain autopsy, the county coroner was stunned to discover that Robin’s brain tissue was overrun with Lewy body proteins. This shocking revelation shows the possible cause of Robin Williams’ tragic suicide.
To understand what the coroner found, Susan enlisted the expertise of Dr. Eric Huang, a forensic neuropathologist and esteemed professor at UCSF. Dr. Huang produced a comprehensive presentation to educate Susan on Lewy body proteins, including detailed slides of Robin Williams’ brain.
“My husband had been dragged through something awful; Dr. Huang pointed out the buildup of tau protein tangles and the amyloid plaque, which is present in Alzheimer’s disease. Then he pointed out the alpha- synuclein, the misfolded Lewy body proteins. I thought, well, wait, you’re telling me my husband did not just have Lewy body disease, but Alzheimer’s and Parkinson’s as well?”
Yes.
Dr. Huang explained that Parkinson’s and Lewy bodies are a spectrum disease and they have the same essential, underlying shared biology. Still, the issue was that, at the time, the Lewy body proteins themselves did not appear in any accurate biomarker. Therefore, when a person is showing Parkinsonism, or Parkinsonian-type symptoms like the shuffling gait, Parkinsonian mask, or cogwheel rigidity, they will most likely be diagnosed with Parkinson’s disease.
Unfortunately, these symptoms were the end of the disease progression for Robin Williams. When he showed these symptoms, his brain was already riddled with Lewy body proteins.
“He had about 40 percent loss of dopamine neurons, and almost no neurons were free of Lewy bodies throughout the entire brain and brainstem,” Susan shares.
She took Robin’s last two years of medical records and full coroner’s reports, which she combed through with her father, who is a retired pathologist. Then, she sent the reports to four medical professionals specializing in Lewy body dementia, because she wanted to get an assessment of Robin Williams’ diagnosis. They all came back and agreed that this was one of the worst cases they’d ever seen of Lewy body dementia. They couldn’t believe he was functional at the time of his suicide.
“Robin was running on fumes. He was filming back-to-back movies and shows, but I believe his Juilliard training helped him keep his composure through the destruction of his mind.”
Susan goes on to share how Robin’s wit and intelligence helped him manage the symptoms: “Robin had such cognitive reserve, and this is a significant point, because I often hear people say, ‘Oh, my father was so smart, and my mother was brilliant, and then it seemed like everything happened so fast.’ That was the case with Robin; it felt like everything happened so fast. First, Lewy body dementia is fast, the lifespan is generally five to eight years, and there’s no cure. Many people don’t even have time to get a diagnosis.”
Since Robin had so much cognitive reserve, this was the key for him. He staved off the symptoms longer than most, but then it was like the dam suddenly broke, and he couldn’t hold back the symptoms any longer. It appeared as though his decline were more rapid, but it actually wasn’t. He’d been declining all along. In fact, he might have had a 15-year prodrome phase, because he could create new neural pathways in his brain.
Susan shares, “Robin had a beautiful mind. He had a lot of roadways in his brain, and I’m sure he used all of them to navigate his world. Robin was freaking amazing and could hang in there longer than most. He was protecting everyone close to him, everyone he loved. He protected us by trying to act normal and not reveal his symptoms. In the end, I believe he took this disease before the disease could take any more of him.”
DIFFERENTIATING DEMENTIAS
The term dementia originates from the Latin words de, meaning “without,” and mens, meaning “mind,” which combined means “without mind.” In Roman mythology, Mens or Mens Bona, also known as “Good Mind” in Latin, was a deity that personified the power of thought, consciousness, and the mind itself. Mens Bona represented the essential quality of “right thinking” to guide Romans toward wise decisions and virtuous actions.
So, when someone begins to lose their right thinking or judgment on a clinical level, they are often diagnosed with dementia.
But what is dementia?
Dementia is a medical condition that involves a significant decrease in cognitive function, leading to difficulties in everyday activities. The primary cause of dementia is Alzheimer’s disease which is characterized by memory loss and cognitive impairment.
David Eagleman is a renowned neuroscientist at Stanford University, bestselling author, and co-founder of innovative startups Neosensory and BrainCheck. As director of the Center for Science and Law, a national nonprofit institute, he brings his expertise on sensory substitution, time perception, brain plasticity, synesthesia, and neurolaw to the forefront of medical research. He clarifies the term dementia: “Dementia is a general term; there are many different flavors, and traditionally, we haven’t been able to distinguish what type someone has until autopsy. And the whole game has been to discriminate earlier between the types, so we can apply the right preventative measures or medical support.”
Dr. Ronald Petersen is a neurologist and the director of the Mayo Clinic Alzheimer’s Disease Research Center and the Mayo Clinic Study of Aging. With his vast expertise and experience, he is committed to leading cutting- edge research dedicated to finding solutions to the challenges of Alzheimer’s disease and aging.
He explains how different types of dementia operate in the brain: “In Alzheimer’s disease, there’s a general network of structures that are involved, and when you look at what those networks do, they are often involved with memory, learning, problem-solving, and language. In Parkinson’s disorders, the alpha-synuclein forming the Lewy bodies often has a predisposition for nerve cells which are in the motor parts of the brain. So rather than the memory and thinking parts of the brain, they’re more motor control. Hence Parkinson’s disease is more motor disorders, coordination, and movement. But the Lewy bodies get into the memory and thinking parts of the brain and the motor parts. So, a typical patient with Lewy body dementia will have cognitive impairment as well as motor problems, so there’s a combination of the two.”

While there are many other causes of dementia, the one that Robin Williams suffered from is called Lewy body dementia, which has the same root cause as Parkinson’s disease.
Let’s start with Parkinson’s disease. Parkinson’s is considered a movement disorder because it affects movement and causes tremors, slowness, and stiffness. In Parkinson’s the alpha-synuclein protein changes shape and clumps up and forms deposits in cells called Lewy bodies in the part of the brain responsible for creating dopamine. These clumps are what researchers think play a role in damaging or causing the loss of the cells that make dopamine, which is responsible for movement.
Robin Williams suffered from Lewy body dementia, and his symptoms were a combination of both mental and physical. A misfolding of the alpha- synuclein protein is present in both diseases. It is a normal protein in our bodies, but with those suffering from Parkinson’s and Lewy body dementia, something goes awry.
Dr. David W. Dodick, MD, FAAN, is an esteemed medical professional renowned for his expertise in the field of neurosciences. He is a trusted authority as a Professor Emeritus at Mayo Clinic and Consultant for Mayo Clinic International. Additionally, Dr. Dodick is the Chief Science Officer and Chair for the Atria Academy of Science and Medicine and an Adjunct Professor at the Norwegian University of Science and Technology. He discusses the impact of Parkinson’s dementia on society: “Parkinson’s disease is probably the fastest growing neurological disease, if not medical disease, on the planet. According to some recent literature, there’s up to a 500 percent increase in the incidence of Parkinson’s disease just over the recent past. Some of that is linked to industrial solvents used in everything from dry cleaning to pesticides to even drinking water. We’re able to see the signs of the disease on brain imaging studies for Parkinson’s disease right now and hopefully with Lewy body dementia, which is what Susan’s initiative is focused on, specifically finding a biomarker for Lewy body dementia.”
“When you’ve gone to the gates of death and you turn around and you look back, life looks pretty different. It becomes a lot less about you and more about what I can do to help others.”
Dr. Rachel Dolhun is a neurology and lifestyle medicine physician specializing in movement disorders and senior vice president of medical communications at The Michael J. Fox Foundation. She points out some subtle differences between Parkinson’s and Lewy body dementia:
- Parkinson’s and Lewy body dementia are both progressive diseases involving brain cell loss and a shared pathology of abnormal alpha- synuclein protein clusters called Lewy bodies.
- Cognitive changes can occur in Parkinson’s, ranging from subtle to more significant changes later in the disease.
- Lewy body dementia is used as an umbrella term for two related conditions: Parkinson’s Disease Dementia and Dementia with Lewy Bodies.
- Parkinson’s Disease Dementia, if it occurs, typically happens after living with Parkinson’s for many years or decades, while Dementia with Lewy Bodies has memory and thinking changes early in the disease at the same time or within a year of the movement symptoms.
- The challenge with these similar diseases is they share many symptoms and don’t yet have a test that can, on its own, tell them apart.
WHAT TRIGGERS THE FOLDING OF PROTEINS?
As a medical professional specializing in aging, Mayo Clinic neurologist Dr. Bradley F. Boeve, M.D. has an extensive range of clinical and research interests, focusing on disorders that lead to cognitive impairment, dementia, and prion disorders. Dr. Boeve’s expertise includes neurogenetics and neurological sleep disorders. His research is focused on various disorders, including mild cognitive impairment, Alzheimer’s disease, Lewy body dementia, and others.
“Lewy body dementia is triggered by the misfolding of alpha- synuclein proteins that clump together, forming what’s known as a Lewy body. This clumping occurs in nerve cells, specifically in the dendrite and axon branches, and fuses into a ball in the cell body. Doctor Lewy discovered this phenomenon in 1912, but we still don’t fully understand the triggers that cause this misfolding.”
He continues, “These Lewy body masses were thought to occur mostly in the brain and particularly in the base of the brain involved in motor functioning. Lewy bodies were discovered in people with Parkinson’s disease, specifically in the part of the brain responsible for dopamine production and movement. This discovery helps explain the symptoms associated with Parkinson’s disease. What has become apparent over many years is that these Lewy bodies are not only happening in various parts of the brain, but they can also happen in the spinal cord and the peripheral nerves—so, the nerves that go to the heart, the GI system, the bladder, and the sex organs. So, what was initially thought to be a brain-related problem has turned out to be a widespread nervous system problem.”
The widespread deposits of protein clumps throughout the body are the reason that Lewy body dementia patients suffer from up to 40 different symptoms as it relates to the disease. There are cognitive symptoms, there are neuropsychiatric symptoms like depression, anxiety, and hallucinations, and there are motor symptoms. There can be what is called autonomic symptoms which are more related to the changes in the body’s nerve cells that can cause constipation and lightheadedness when a person stands. Lewy body dementia can also cause urinary incontinence and erectile dysfunction. It also affects several sleep circuits, so that numerous sleep issues can happen. Abnormal Lewy bodies can affect the olfactory bulb, causing it to degenerate, and patients may have difficulty detecting smells.”
Dr. Dodick clarifies, “By the time diseases like Parkinson’s are diagnosed, the brain has already suffered significant damage. Eighty percent of the dopamine-containing cells in certain brain areas have already been depleted. This means that symptoms are already present before a diagnosis even takes place. Telltale symptoms and signs that may not be recognized by the individual or by family members or friends can occur, but signify to a physician that they may be in the earliest prodromal phase of Parkinson’s disease or Lewy body dementia, even though they don’t have any symptoms yet—symptoms like REM sleep behavior disorder, where people move during REM stages of sleep. Normally when you’re dreaming, you’re paralyzed. So, if you’re moving during the dream phase of sleep, that’s abnormal. This behavior disorder, where people thrash or move about during dream sleep, is a telltale sign of Lewy body dementia.”
To make life even more complicated, the diseases do not exist in isolation; sometimes, doctors find a combination of all three, as with Robin Williams.
Lewy body dementia affects over 1.4 million Americans, making it a prevalent medical condition. While it is the second most common form of dementia, Alzheimer’s remains the largest contributor to the current 5.7 million people estimated to be affected.
LBD HALLUCINATIONS
One of the common symptoms of dementia with Lewy bodies is experiencing hallucinations, including nonvisual ones like hearing music and auditory ones that may be threatening and trigger feelings of persecution. Additionally, patients may experience delusions, such as believing that people they know and love are impostors in disguise. These core clinical features are enough for a doctor’s diagnosis of probable dementia with Lewy bodies.
Susan shares, “I asked a client of mine who was recently diagnosed with Lewy body dementia how she was able to get a diagnosis, and she says it was the hallucinations. Having hallucinations was the one symptom Robin would not share, and I completely understand why. He was already experiencing anxiety through the roof. His amygdala was broken. His brain had lost the ability to temper and adjust his sense of apprehension. Fear and paranoia took over. In Robin’s brain, one of the worst deposits of Lewy body proteins was in his amygdala, so there was no proper communication happening.”
The amygdala plays a crucial role in processing threatening or fearful stimuli. It is responsible for detecting impending danger and triggering fear- related responses. Essentially, it is the core apparatus of a neural system that helps us to stay safe. But in Robin Williams’ brain, the Lewy body proteins took control of the mainframe and set off false alarms that he was in danger and bad things were happening when nothing was happening in real life.
As a medical expert, Dr. Ronald Petersen sheds light on the reason behind visual hallucinations in Lewy body dementia patients, “Interestingly, the location of Lewy bodies and affected nerve cells in the brain tends to be in the visual-spatial areas, leading to a pathology-location correlation. This indicates that Lewy body dementia patients experience hallucinations due to the Lewy bodies mainly affecting the visuospatial part of the brain, which includes the perioral and occipital areas. Our vision enters the eyes and projects back to the occipital part of our brains, while the parietal part is involved in spatial orientation. Hence, when Lewy bodies disrupt the visual- spatial area, things can get out of hand and cause hallucinations.” Another potential mechanism could relate to the Lewy bodies affecting the circuits in the brain involved in REM sleep control. Dr. Boeve explains, “We know that REM sleep behavior disorder – a sleep disorder in which individuals seem to ‘act out their dreams’ – often precedes the development of dementia or parkinsonism in those with Lewy body disease. This sleep disorder reflects aspects of wakefulness invading into REM sleep. The opposite may also be happening – aspects of REM sleep such as dream-like imagery could be invading into wakefulness and contributing to visual hallucinations.”
Susan’s client, who has Lewy body dementia, shared an episode with her. She said she knew her husband was in the room with her, and he was sitting on the couch, but then she saw a ghost of him in the corner. She was fine when the ghost didn’t move, because she knew what was going on, but when the ghost started to move, that’s when it got hard.
Dr. Bruce Miller is a respected medical expert in neurology and a distinguished professor at the University of California, San Francisco. As the director of the Memory and Aging Center and the founding director of the Global Brain Health Institute, Dr. Miller is committed to advancing research in the field of brain health. He also plays a pivotal role in leading two prominent collaborations, the Tau Consortium and The Bluefield Project, focused on precision medicine to develop treatments for tauopathies and progranulin-mediated forms of frontotemporal dementia. He explains hallucinations from a patient’s perspective: “We always ask if the patient feels like there is a presence lurking behind them. Maybe they can’t quite see them, but this is widespread first evidence. Some people get illusions initially. I think they come from the part of the brain where we conceptualize faces, people, and animals. One of my favorite patients saw spiders making webs in his bedroom, and I got him on the right medication. After that, he put a fan in the room and said that the fan got rid of the spiders and their webs. So, I think they can be malleable to treatment. Sometimes people enjoy them. Some people are terrified by them. So, the emotional response varies a fair bit.”
When Susan speaks about Lewy body dementia around the country, she clarifies that hallucinations, while they’re very hard to talk about, are one of the hallmarks of the disease.

HELPING OTHERS THROUGH ROBIN’S WISH
Susan recounts more of the conversation with her client suffering from Lewy body dementia, whose husband had requested a commissioned painting for them. During their hour-long conversation, the client gave Susan important insight into the disease. She likened having Lewy body dementia to holding a live grenade without knowing when it would detonate or the damage it would cause. This analogy highlights the uncertainty and fear that comes with Lewy body dementia.
Living with hallucinations and paranoia was a conversation Robin and Susan never got to have. She was in the trenches with him, but had no idea about his hallucinations.
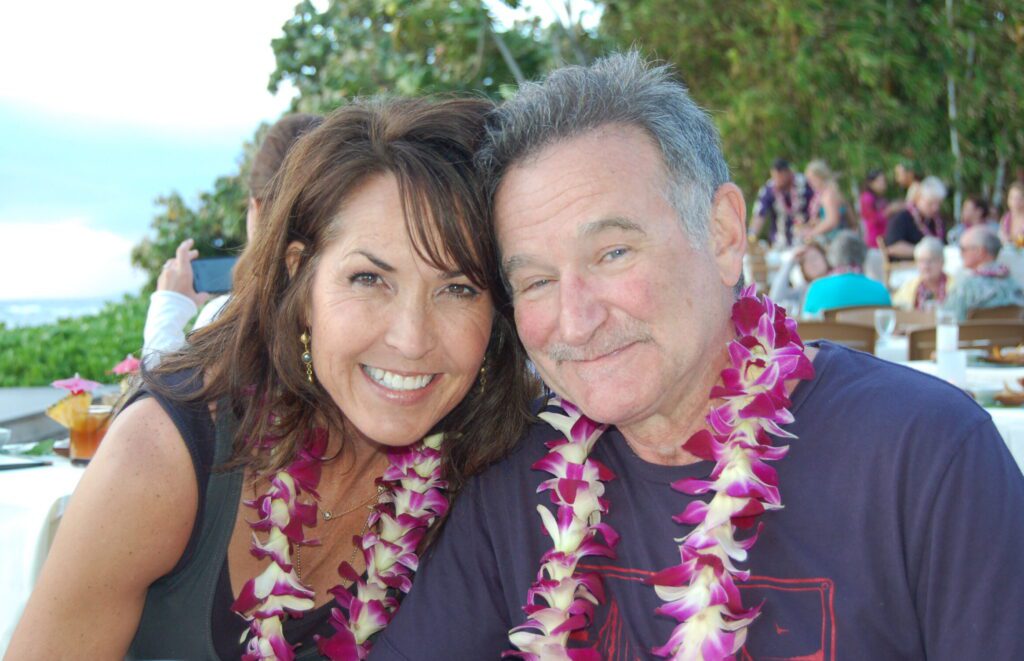
There were so many unanswered questions before Robin died. Once Susan dug into the findings of the autopsy report she felt it was her responsibility to share their story. Participating in the film Robin’s Wish was one means to do that. The film project took over five years but Susan knew their story could help spread awareness and raise support for LBD. The documentary helped to fight the many misconceptions about Robin’s state of mind and stigmas of mental illness. The film brings awareness to a disease while all too common is still unknown to many. Robin’s Wish premiered on September 1, 2020 to critical acclaim. Susan rolled up her sleeves to tell the true story and rewrite his legacy. For fans around the world, the complete story of what really happened to Robin was finally told.
DOPAMINE’S ROLE IN THE BRAIN
Ironically, in the blockbuster movie Awakenings, Robin Williams played Dr. Malcolm Sayer, a physician at a hospital in the Bronx, who discovered that certain stimuli could reach beyond the catatonic states of patients who survived the encephalitis lethargica epidemic. Simple actions like hearing music, catching a ball, and being touched by a human have unique effects on individuals. After attending a conference on the success of L-DOPA for Parkinson’s patients, Sayer (played by Williams) believes the drug can also help his patients. After a successful trial with catatonic patient Leonard Lowe (played by Robert DeNiro), Sayer seeks funding to provide L-DOPA to all catatonic patients and grant them “awakenings” to reality.
This breakthrough had the potential to change the lives of many patients. Unfortunately, L-DOPA was insufficient to keep the patients from a catatonic state. This movie was based on the true story about the work of Dr. Oliver Sacks, whom the New York Times heralded as “The Poet Laureate of Medicine.” Dr. Oliver Sacks was a physician, best-selling author, and professor of neurology.

Susan recalled a profound conversation she had with a young neurologist that she met at the National Institute of Neurological Disorders and Stroke (NINDS) during the filming of Robin’s Wish, “This young gentleman in his lab coat told me that it was because of Robin’s role in Awakenings that he got into neurology in the first place and now here he was working on the very disease that Robin got.”
Dr. Boeve explains there’s a small part in the base of the brain called the substantia nigra. That is the central part of the brain that makes dopamine, which has branches that go to various other parts of the nervous system and the nerves that produce dopamine. Dopamine is the primary neurotransmitter involved with movement. The symptoms are complex, but tremors, shuffling gait, and stooped postures are apparent when a patient is low on dopamine. Many of the symptoms are classically related to features of Parkinson’s disease.
Dr. Petersen further clarifies, “The presence of Lewy bodies in the brain can often lead to a deficiency in the neurotransmitter, dopamine. This deficiency is common in Lewy body disorders, including Parkinson’s disease. Patients suffering from these disorders may benefit from dopaminergic drugs which increase the amount of L-DOPA in the brain. Additionally, when hallucinations occur in diseases like dementia with Lewy bodies, psychiatrists and medical practitioners utilize dopamine blockers.”
It’s worth noting, however, that excessive dopamine levels may create hallucinations, but traditional dopamine blockers can potentially harm patients already deficient in dopamine. Therefore, great care should be taken in their administration.
Susan shares, “Robin had a panic attack, and his doctor recommended an antipsychotic medication to help with the anxiety. It made things better in some ways, but far worse in others. Not until he left us would I discover that antipsychotic medications often worsen effects for people with Lewy body dementia. Also, Robin was highly sensitive to medications, and sometimes his reactions were unpredictable. Later I learned this is a common theme in people with Lewy body dementia.”
Melissa Nerenberg’s article in Neurology, titled “Lewy body disease and suicidality after dopamine agonist withdrawal” (October 24, 2016) about Lewy body disease and the connection between suicidology and dopamine speaks to why it is we must have accurate biomarkers to diagnose Lewy body dementia correctly. If you give someone with Lewy body dementia an antipsychotic, it can speed up the disease progression, and then when the antipsychotics are discontinued, the disease progression can remain.
Not only that, but it can also cause the total opposite of what the drug was intended to do. For example, suppose someone with Lewy body dementia has a psychotic episode. In that case, they might end up at the emergency room, and the doctor might first prescribe antipsychotics, yet that can be the most dangerous measure for someone with Lewy body dementia.
“I went through this experience with my best friend, my husband, the love of my life. We were drowning on these class-5 rapids, not knowing what direction we were going to get tossed. I’m experiencing all this from my perspective, not knowing about his hallucinations and overwhelming fear, then I pop out the other side, but Robin didn’t make it.”
She continues, “Robin’s brain had become putty. His neurotransmitters were not working. The chemical messengers were not conveying what they were supposed to do. Now I know that one of the classic symptoms of Lewy body dementia is delusional looping. That’s when we no longer had a break between day and night. Sometimes when Robin got into a delusional loop, I didn’t know if it would last three hours or three days. It was terrifying and exhausting. You live between two worlds, fiction and nonfiction, and you’re trying to rescue your partner from the fictional world, but they don’t know the difference. One thing I learned about suicide is that there’s always more to it. Always more, and you cannot possibly judge what’s happening in a person. Not even close.”

Susan shares what happened days before Robin left us: “The pressure was on. We were supposed to decide what inpatient neurocognitive testing facility he would go to the week he took his life. Robin didn’t want to be locked up. I believe that if Robin was hallucinating, he didn’t think he would ever be able to come out again.”
“Robin did not die of depression. Depression is one of the 40 symptoms of Lewy body dementia.
We were together for seven years, and my husband was not depressed.”
-Susan
RESEARCH
“If we had a proper diagnosis, Robin could have started to take his power back. Instead of trying to figure out what was wrong, we could have planned our future. Like, hey, honey, you want to go hang out on a beach, or do you want to fight this disease? Do you want to give money to research, or do you want to be part of clinical trials? There are ways you can have power over Lewy body dementia, and I’ve taught this to other families suffering through this horrific disease,” Susan explains.
Research is progressing rapidly with the recent groundbreaking discovery that The Michael J. Fox Foundation announced in April 2023. Through The Michael J. Fox Foundation’s landmark brain health study, the Parkinson’s Progression Markers Initiative (PPMI), a new tool has been discovered that identifies an essential pathology of Parkinson’s disease in living people: abnormal alpha-synuclein in brain and body cells. This discovery represents a giant leap forward in researchers’ ability to identify and understand the disease and offers hope for improved care and treatments. The tool, called the α-synuclein seeding amplification assay (αSyn-SAA), can detect pathology in spinal fluid not only of people diagnosed with Parkinson’s, but also in individuals who have not yet been diagnosed or shown clinical symptoms of the disease, but are at a high risk of developing it.
This breakthrough is ready to transform clinical trials, making them faster and cheaper. And, in the future, it will hopefully help transform diagnosis, care and, ultimately, help prevent disease, too. Because this tool cannot yet, on its own, diagnose or predict individual diseases, it’s best to speak with a movement or cognitive expert to learn what it can and can’t tell you and whether it might be helpful in your individual health journey. Susan has been working with the American Brain Foundation (ABF), hoping to find a biomarker to help diagnose Lewy body dementia while someone is alive.
“The research team will update me at the end of summer, and I can’t wait to see and talk with them about their progress. If we can get the blood plasma biomarker to work and be accurate, that will be much easier for clinicians everywhere to access in less time,” Susan shares with excitement.
Her friend, Ted Turner, has LBD. At the Lewy Body Dementia Association’s (LBDA) request, she painted a breathtaking scene from his property in Montana, and she had a chance to talk with him about his diagnosis. In preparing for her visit with him Susan Schneider Williams recalled thinking “How prescient was Ted back in the day? All he wanted to do was make his money to save our environment and the planet, which would in effect save our brains.”

PREVENTION
Dr. Eagleman explains why it can be challenging to get diagnoses before preventative measures can be implemented, “Somebody hits a stage of mild cognitive impairment when things are starting to get a little bit diminished. But typically, what happens is that people say, ‘I haven’t been getting enough sleep, or I’m feeling stressed.’ Everyone has excuses for feeling less sharp. Often by the time they see a doctor for their symptoms, it’s too late: dementia has already set in.”
Dr. Dodick believes slowing down the progression of neurodegenerative diseases like Parkinson’s is possible through lifestyle changes. Exercise is effective in slowing down the progression of Parkinson’s disease. For example, with objective quantification of factors like gait, sense of smell, and sleep, the risk of developing these diseases can be detected early on or before symptoms appear.
Delaying the onset of these diseases is critical because once symptoms appear, most brain cells are already damaged beyond repair. Therefore, preventing the onset will have a more significant impact than trying to delay the progression of the disease.

To achieve this, Dr. Dodick suggests adopting a medically backed eating plan, such as MIND, which can enhance cognitive function and ward off age-related brain issues. The MIND diet is designed to support a healthy brain. Its name stands for Mediterranean-DASH Intervention for Neurodegenerative Delay, and it merges critical elements of the DASH diet (Dietary Approaches to Stop Hypertension) and the Mediterranean diet. The MIND diet helps enhance cognitive function and lower inflammation by emphasizing specific food groups featured in these diets. “To optimize my health, I’d incorporate aerobic and resistance training into my routine. I’d prioritize getting at least seven hours of quality sleep each night and ensuring my diet supports my fitness goals. In addition, I’d focus on mindfulness and stress management techniques to increase my vagal tone and reduce my stress levels. This would involve daily breathing exercises three times a day and a mindful approach to these practices.” Dr. Dodick shares.

COGNITIVE FITNESS
Dr. Eagleman explains that cognitive fitness is one of the best ways to keep your brain healthy. He explains, “Pushing your brain so that it’s doing the hard work of learning new things is essentially the best thing we know to prevent the ravages of any flavor of dementia. And the reason is brain plasticity, which is building new bridges and roadways even as parts of the brain are falling apart. Somebody who retires and sits on the couch watching television would have been much worse off than Robin. Robin was the guy who had a million ways of working his brain constantly with memorizing scripts, playing different characters, traveling, biking, and doing stand-up comedy.”
Dr. Eagleman continues, “Cognitive fitness is about pushing your brain. It’s much like going to the gym. You won’t get stronger if you work out but do the same thing every time. You get stronger at the gym by constantly surprising your muscles, doing things you haven’t done before, and pushing yourself. You have to keep yourself between the levels of frustration and achievable. Figure out how to do things that are hard for you. Once you get good at crossword puzzles, then switch to Sudoku. As soon as you get good at Sudoku, quit doing that and do something that you’re no good at. That is the key. Constantly seek novelty. One thing I try to do, by the way, is to drive a different route home from work every day. It doesn’t take much longer, but it opens up my mind. The one thing I always have done is switch which hand I brush my teeth and shave. Things like switching up your office are easy to do. For example, switch your books on your bookshelf once a month or move your artwork around. People want comfort and familiarity, so you must force yourself to do this. But it’s so worth it in the name of cognitive fitness, because it forces your brain off the hamster wheel and propels you to do something differently, keeping your brain fit and healthy.”

SUSAN’S ADVOCACY
Although she had the choice to depart into the shadows after Robin’s tragic passing, Susan bravely remained amid the trauma to convey an important message about Lewy body dementia. Her unwavering commitment to spreading this message is why she chose to stay within those painful experiences. Susan is commended for her bravery and resilience in such adversity.
So many people come up to her and say, “I’m a doctor in this small town, or I’m a doctor here,” and the conversation about Lewy body dementia is in that room because of Susan Schneider Williams and her advocacy work. Now, something that no one ever heard of is suddenly part of the conversation across America. People are grateful to Susan Williams for making Lewy body dementia a mainstream issue. It’s a conversation that is happening in private homes and doctors’ offices around the country, and they are talking openly about the symptoms without shame. That is incredible progress.

Susan was at the recent American Academy of Neurology conference in Boston as the Lewy body ambassador for the American Brain Foundation. A neurologist pulled Susan aside and said, “I just want to thank you for the film, Robin’s Wish. I can’t tell you how many times I’m giving a patient the diagnosis and I’m able to tell them, you know, this is what Robin Williams had. This film will help you. This information will help you.”
“I hoped my advocacy would help raise the conversation and educate. I wanted the film to be a tool doctors could use to comfort patients, letting them know they’re not alone. Joseph Campbell says that you must be willing to ditch the life you thought you would have for the one intended for you,” she shares.
For her, it also goes back to purpose. Since she was 20 years old and decided to become clean and sober, Susan has dedicated her life to being a vehicle for good. No matter how bad it got or how much shame could be caused, she stepped up and became a beacon of light for others who also suffered in silence.

“Whatever your fear or shadow is, there’s no point in being ashamed. It is your most prized possession, because from that you can use it as a launchpad. Every day I ask how can I take my experience and help someone else?”
“The light is what attracts me to a subject. The studio has always been a lab to me. It’s where I get to explore the true elements of a composition. It’s where I can make observations and problem-solve as I try to convey with paint the message of a moment in time. Through it all, the more I learn about my subject, the more I learn about myself.”

THE FUTURE FOR SUSAN
“I got the information and urgency out about Lewy body dementia jump started, and now I can return to painting. Robin loved watching me paint; we were just two artists sharing space for our time. I’m just so grateful that I don’t have to take myself back to that place of trauma all the time anymore. It was tough for years, but now I can hand off the baton to the neurologists and to Robin’s Wish,” Susan says. She continues, “I’m so grateful that I’ve gotten to play a role in helping to align the many consulting partners for Robin’s Wish and supporting SPARK, the educational version of the film. My work at the American Brain Foundation, where I was on the board for six years, the last four of those as vice chair, also involved bringing people and organizations together—plus a lot of strategy work. I helped establish the Lewy Body Dementia Fund and spearheaded a $3 million research award targeted at finding an early biomarker for Lewy body dementia. What’s so exciting about this grant award is that it is also built on bringing together different organizations and researchers from different fields to help fix the problem. After experiencing Lewy body dementia up close and not knowing what it was, I wanted to learn the science behind it. Now I’m the Lewy body dementia ambassador at the ABF.”
When thinking about her future, Susan shares, “I’m looking forward to launching my online store, ssfineart.com, where a portion of all print proceeds will support Lewy body dementia and related brain disease research. I’ve really appreciated the extra meaning behind the work that I’ve done lately, for example, the painting for Ted Turner. The LBDA had asked if I would do a painting for him, honoring his work around Lewy body dementia, including how he’s shared his own Lewy body dementia experience with the world.”
The heartbreak of losing a loved one to a mysterious illness is immeasurable. Susan’s journey with her husband was painful, but through her tragedy, she discovered the importance of understanding medical conditions like Lewy body disease. Though it was too late for Robin Williams, she hopes her story might help others facing similar situations.
As dreadful as it has been, she has given meaning and purpose to Robin Williams’ death. She could have hidden away from the world, but she took a brave step forward to uncover what took the life of this effervescent soul who brought us so much happiness. Because of her tireless investigation, she found that Robin’s brain hid the clues to his death and his killer was embedded in the slides of his autopsy. From there, she led a crusade to understand this silent killer and lift the shame through sharing symptoms that might be frightening or confusing.
Susan leaves us with one last memory of him. “One quiet morning, I asked, ‘Robin, when we get to the end of our lives and look back, what do you want your legacy to be?’ I couldn’t believe how fast he answered.
Robin said, ‘I want to help people be less afraid.’”
Susan, through your work, you have fulfilled Robin’s wish. You are helping people to be less afraid.
Thank you, warrior princess.
If you or a loved one is suffering from any symptoms in this article, please contact your primary care physician and ask to see a neurologist who has expertise in Lewy body dementia.
For more information about Lewy body dementia, visit lbda.org, michaeljfox.org and americanbrainfoundation.org